Improve Implant Reimbursement: 7 Revenue Cycle Strategies
Implants are standard in many surgical procedures in the outpatient setting, but they are notorious for being one of the most expensive components of any surgery, as well as one of the most challenging in terms of capturing reimbursement. From patient intake to claims management and managed care contracting best practices, here’s our top revenue cycle strategies that improve the rate of collections on implants.
1. Streamline Revenue Cycle Processes: Front-end Operations
Most claim errors can be traced back to front-end operations and the patient intake process. Improving the accuracy of implant claims starts with streamlining revenue cycle processes within front-end operations, such as optimizing how your team collects and stores patient demographics. Utilizing online portals within your practice management software can enable new patients to complete paperwork before appointments, reducing errors and allowing for verification of information upon arrival.
2. Verify Patient Information, Provide Cost Estimates
Verifying patient information is an important step to ensure accuracy in the billing and claims process. Verifying patient demographics, insurance coverage and benefits can also help your team produce copay estimates and notify patients of their financial obligations. Providing payment details ahead of time minimizes unexpected out-of-pocket expenses. The more prepared patients are to pay for the procedure, the more likely you’ll receive timely payment.
3. Obtain Prior Authorizations for Implant Procedures
Securing prior authorizations for surgical procedures is essential for both patient coverage and ASC reimbursement. Always confirm with the carrier whether a procedure requires prior authorization as well as what documentation is necessary to mitigate the risk of revenue loss due to claim denials.
According to AMA surveys, an overwhelming 88% of physicians express frustration with the administrative burden associated with prior authorizations. The prolonged turnaround time poses a significant obstacle, particularly for patients in need of immediate medical procedures.¹ Fortunately, leveraging automation can alleviate these challenges.
Chart management software offers cost-effective solutions to streamline a variety of revenue cycle processes, including automating chart pack preparation to expedite scanning and printing tasks often required for prior authorizations.
This software can also seamlessly integrate with scheduling, transcription, and billing solutions to provide real-time insights into case statuses and facilitate prompt documentation retrieval as needed, all from a single user-friendly dashboard.
4. Transcription, Coding, and Billing Practices for Implants
To meet timely filing deadlines, it’s essential to decrease turnaround between dictation, transcription, and coding.
If your revenue cycle integrates transcription, coding, and billing into one workflow, then claims can easily pass to each department and decrease the days to bill, increase your efficiency, and improve your rate of collections.
For example, a user-friendly transcription mobile app can send push notifications to team members, reminding them to e-sign documents or alerting them when a operative note is ready for coding. ASC coders rely on the accuracy of reports and OR notes to ensure compliance with each payer’s specific coding guidelines. It’s critical for corresponding documentation to match what was authorized and what was performed.
For implants, there are codes that indicate the type of implant, the location of the implant, and the reason for the implant. Some implants have their own HCPCS code, others require specific revenue codes to receive reimbursement. Using the wrong code or failing to code the procedure correctly can result in underpayment or nonpayment. Knowledgeable coders ensure each claim aligns with payer coding requirements.
While accurate documentation and specialized expertise is necessary for coders, it’s critical for the billing team to have the right systems for charge posting, claims management, and payment posting. Armed with a specialized knowledge of surgical implant billing requirements and a tech-enabled workflow, your team can successfully track claims, catch errors, and facilitate swift follow-up protocols to appeal denied claims.
5. Analyze Revenue Cycle Patterns to Improve Implant Clean Claim Rates
Regularly reviewing the accuracy of your claims will help you identify common reasons for claim denials. Auditing the reasons for claim issues can also help you notice patterns with a particular implant, payer, or revenue cycle inefficiency.
For example, analyzing your claim denials on a weekly and monthly basis can unveil patterns of error, such as incorrect coding. Once you know where the errors originated, you can adjust accordingly – such as updating outdated codes – to enhance clean claim rates and your rate of collections.
Leveraging data analytics tools can track claim denials by a variety of metrics, and track when your ASC receives implant reimbursement and the amount. These tools can also compare how long it takes to receive reimbursement to the cost of the implant and any other fees associated with the procedure. This will help you identify expenses and monitor cash flow on a case by case basis to track which cases are profitable and where contract negotiations might be needed.
6. Claims Management for Implants
Establishing a high-dollar claims work queue for your accounts receivable (A/R) team can help prioritize and streamline the process of following up on outstanding implant claims. Staff can then prioritize claims based on factors such as the dollar amount, the age of the claim (date of service), and the payer involved.
Establishing clear communication with payers and leveraging technology for streamlined follow-up processes are key components of effective high-dollar claims management.
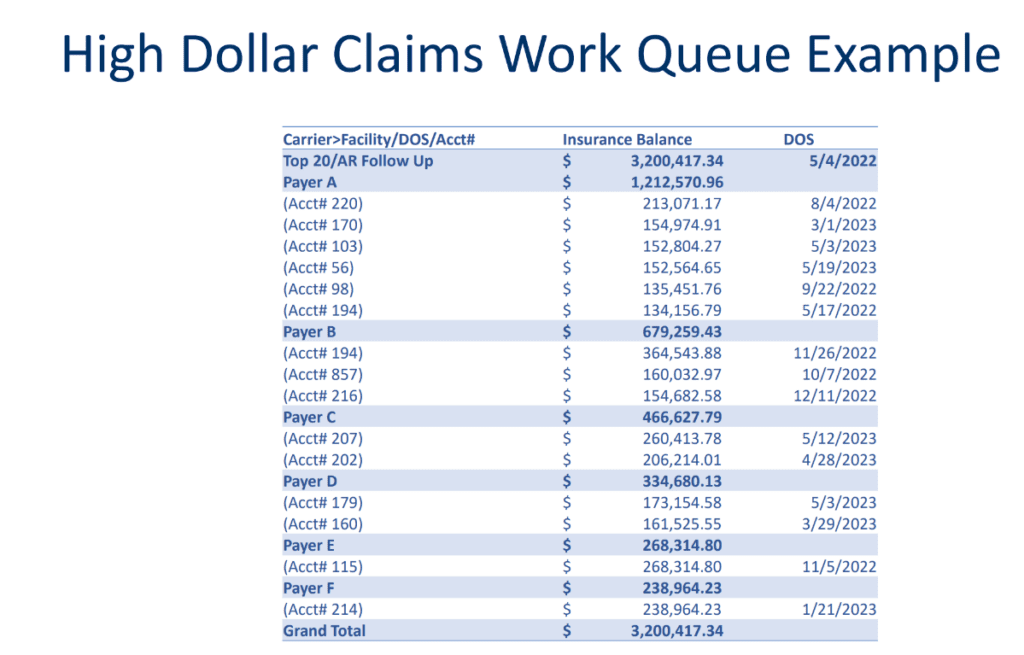
For example, your team can leverage technology to streamline the follow-up process by automating tasks like sending follow-up emails or payment reminders.
If a claim is denied or delayed, your A/R team should be prepared to appeal the decision and follow up appropriately. This may involve providing additional documentation or further communicating with the payer.
7. Managed Care Contracts and Implants
Rely on the terms in your managed care contracts to meet each payer’s requirements for implant reimbursement. Since contracts differ by payer, your implant reimbursement protocols and profit margin will differ by payer.
For example, some payers require a copy of the implant invoice to accompany the claim. Specific documentation may also be required to prove medical necessity and why the implant and the procedure is justified. Contract language also dictates if you can bill using an invoice cost plus structure (meaning you can bill for the implant cost, plus a little extra to cover overhead costs).
If you know a procedure is not profitable because the cost of the implant is greater than a payer’s reimbursement, then that’s often the first step in justifying the need to negotiate better contract terms. You can then analyze if you should negotiate carve-outs for implants instead of a flat fee, since carve outs can cover at least the cost of the implant, plus shipping and handling.
For more information on the relationship between managed care contracts and implant profitability, read this Q&A blog post with our Our Senior Vice President of Managed Care Contracting, Scott Allen.
Improving implant reimbursement starts with revenue cycle best practices. By implementing these seven strategies, ASCs and administrators can increase revenue and reduce the risk of errors and denials on implants.
Are you looking for ways to improve your revenue cycle management? Take the first step towards optimizing your revenue cycle process by requesting a revenue assessment from our team of RCM experts. Request a demo.
References:
- American Medical Association. (2018). AMA Prior Authorization (PA) Physician Survey. https://www.ama-assn.org/system/files/prior-authorization-survey.pdf