ASCs Transform the Outpatient Experience: Lowering Healthcare Costs and Improving Value
Stacie Fults, SVP and Reba Watson, SVP, client services
ASCs have transformed the outpatient experience by offering a convenient and personalized alternative to traditional hospital settings. These centers provide high-quality, cost-efficient surgical care for millions of Americans annually, making them an integral part of the healthcare landscape. With over 11,500 facilities across the country, ASCs provide same-day surgeries that enhance patient convenience and satisfaction.
August is National ASC Month, a time dedicated to raising awareness about the vital role ASCs play in healthcare. During this month, ASC staff and physicians invite key policymakers to tour their facilities, while advocacy groups educate the public about the benefits ASCs offer.
As the leading provider of revenue cycle management (RCM) services to the ASC industry, nimble is at the forefront of advocating for our clients. We focus on improving contract terms and reimbursement operations, ensuring that ASCs get paid more and get paid faster, enabling them to thrive in a competitive market, despite staffing challenges and rising costs.
Top 10 Facts to Know About ASCs
Patients have more choices now than ever before when selecting their surgical provider. They are focused on the value and quality of care they receive. Their financial responsibilities also play a role in their decisions due to healthcare costs and the prevalence of high deductible plans.
Here are the top ten differentiators and how ASCs are transforming the outpatient experience, improving the value of surgical care while lowering costs:
1. Specialization: ASCs focus on specific types of procedures, offering specialized care and expertise.
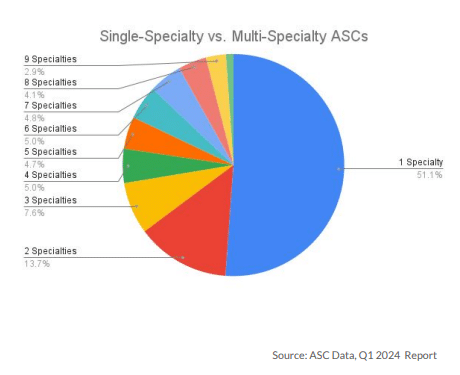
Today, approximately 51% of ASCs are single-specialty, and 49% of ASCs are multi-specialty
Endoscopy and ophthalmology are the top two specialties for single-specialty ASCs, and most multi-specialty facilities focus on orthopedic and pain management procedures.
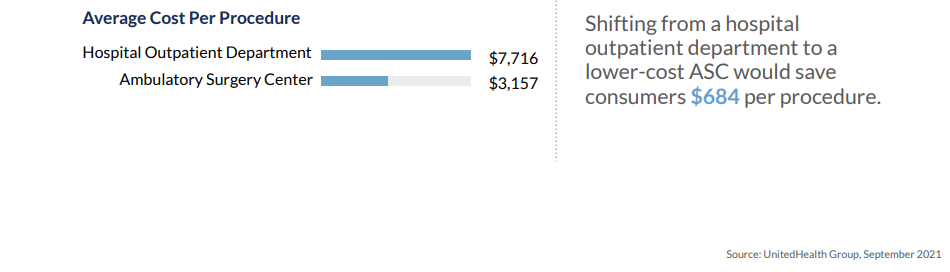
2. Cost Savings: ASCs typically offer lower-cost procedures compared to hospital outpatient departments due to reduced overhead and operational efficiency.
3. Better Surgical Outcomes: Procedures at ASCs are done on an outpatient basis, meaning patients go home the same day, which can reduce the risk of hospital-acquired infections and improve surgical outcomes.
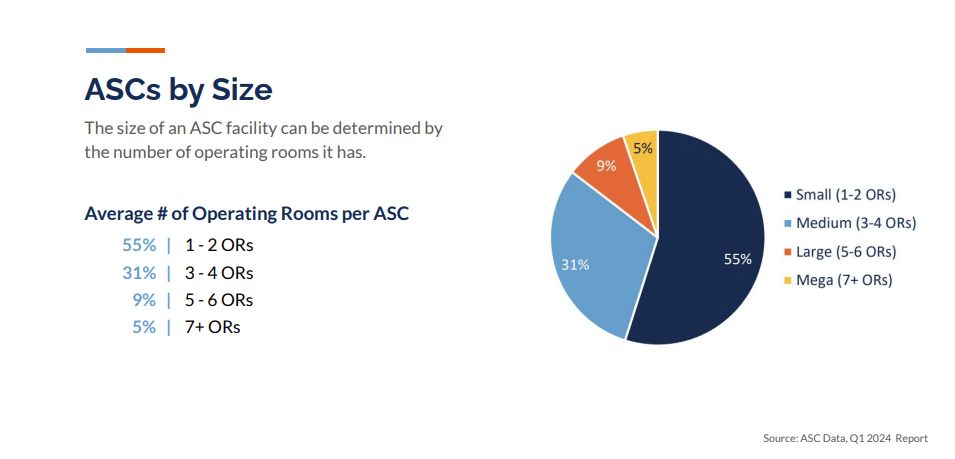
The average ASC has one to two operating rooms, while some hospitals have 85. A facility’s total number of ORs can indicate its ability to handle multiple operations simultaneously; however, with the number of hospital patients recovering overnight in larger facilities, the chances of post-surgical infections can increase. ASC patients are less likely to be admitted to the hospital for post-surgery complications or infections, and their recovery time is faster compared to in-patient care.
4. Efficient Operations and Patient Satisfaction: Designed for efficiency, ASCs streamline processes, reduce wait times, and improve patient flow, leading to higher patient satisfaction and a better overall experience.
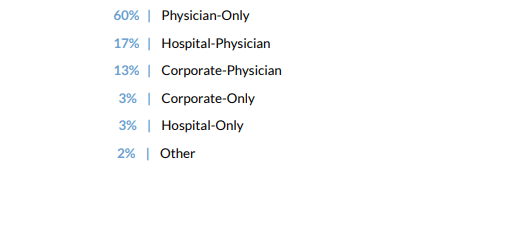
5. Physician Ownership: Most ASCs in the US are owned by the physicians who work there, providing a unique perspective and commitment to patient safety, cost management, and operational efficiency.
6. Regulatory Compliance: ASCs adhere to strict state and federal regulations, ensuring quality and safety. They undergo regular reviews to maintain these high standards.
7. Innovation: Many ASCs are early adopters of new technologies and minimally invasive procedures, enhancing patient outcomes.
8. Value-Based Care: ASCs align well with value-based care models, focusing on quality and outcomes rather than volume.
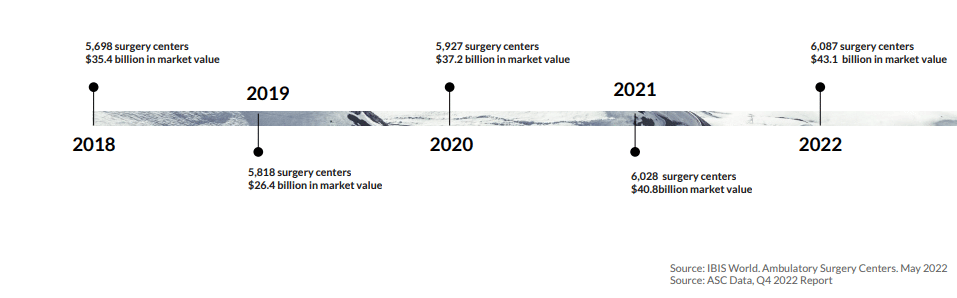
9. Growth Trend: The number of ASCs is increasing as more procedures move from inpatient to outpatient settings.
In the past decade, the number of ASCs has expanded by 15%, saving Medicare approximately $4.2 billion annually.
10. Health System Partnerships: With rising healthcare costs, health systems increasingly recognize the value of ASCs.
Many hospitals are converting their outpatient surgery departments to ASCs, optimizing cost-efficiency and profitability. Due to changes in CMS reimbursement, many cardiovascular facilities are opting to operate as ASCs and as office-based labs (OBLs). It’s clear that developing partnerships with ASCs is becoming central to the overall financial strategy of extensive healthcare service networks. This trend is expected to accelerate as more procedures are approved for the outpatient setting and hospitals continue to look for ways to reduce costs.
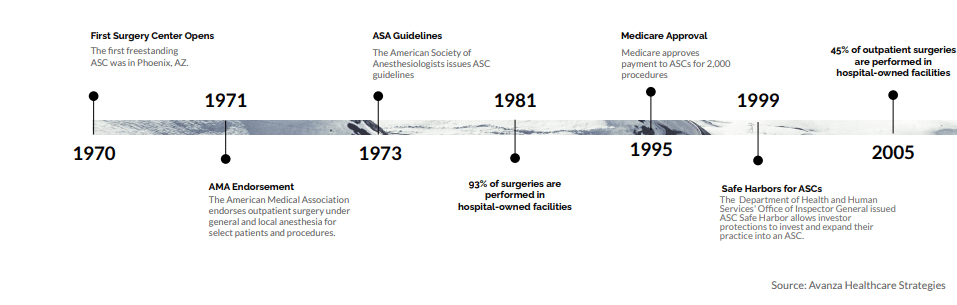
The History of ASCs
The first ASC opened for business on February 12,1970, marking the beginning of a significant shift in the surgical landscape.
The ASC market has since experienced substantial growth, driven by the COVID-19 pandemic, technological advancements, and regulatory changes allowing more procedures in outpatient settings.
As we look ahead to the future of healthcare, see how the ASC industry as evolved and grown since 1970 to present day here.
How nimble Secures the Success of ASCs in the Healthcare Ecosystem
nimble plays a crucial role in ensuring the success of ASCs by providing tailored solutions that address the unique needs:
- Streamlined Revenue Cycle Management: nimble’s specialized, tech-enabled, and fully integrated RCM workflow helps ASCs manage their revenue cycle efficiently, from patient intake through transcription, coding, claims processing and payment collection. This streamlined approach reduces administrative burdens and accelerates cash flow.
- Data-Driven Insights: With nimble’s analytics capabilities, ASCs can gain valuable insights into their operations, identify trends, and make informed decisions that enhance financial performance and operational efficiency. These insights put our clients in the driver’s seat to manage and grow their business.
- Regulatory Compliance: From contracting to chart storage, coding and recovering revenue, nimble’s surgical expertise helps ASCs stay compliant with ever-evolving healthcare regulations and payer updates, ensuring that they meet all necessary requirements and avoid potential penalties.
- Technology Integration: nimble integrates seamlessly with existing practice management and EHR systems, providing one cohesive solution that enhances operational workflows and supports growth and success.
ASCs are transforming the healthcare landscape by providing cost-effective, high-quality care in an outpatient setting. Their role in improving value and patient outcomes is vital as the industry shifts towards more efficient and patient-centered care models. As healthcare costs continue to rise and the demand for value-based care intensifies, ASCs are proving to be crucial in addressing these challenges. With support from innovative revenue cycle partners like nimble, ASCs are well-positioned to thrive and drive positive change in healthcare.
Are you looking for ways to improve your revenue cycle management? Take the first step towards optimizing your revenue cycle process by requesting a revenue assessment from our team of RCM experts. Request a demo